About Polycystic Ovarian Syndrome (PCOS)
Polycystic Ovarian Syndrome (PCOS) is a very common hormone problem, affecting up to 5 million US women of child-bearing age. However, this condition can continue far beyond the reproductive years. The National Institutes of Health states that women with Polycystic Ovary Syndrome have at least two of the following conditions:
- Absence of ovulation, which leads to irregular or no menstrual periods
- High levels of androgens, such as testosterone and DHEA (often thought of as male hormones, but women have them as well)
- Cysts (fluid-filled sacs) on one or both ovaries
However, while “polycystic” literally means “having many cysts”, some women diagnosed with PCOS don’t have cysts on their ovaries. What happens over time is that because the ovaries contain follicles, eggs that are released do not make it down to the uterus and be trapped in the follicles. The ovaries appear enlarged because the follicles that surround the eggs look like “cysts.” An ultrasound is usually required to confirm.
Underlying Causes of PCOS
PCOS is a collection of symptoms centered around irregular ovulation. Its causes are hormonal and metabolic, with interconnected symptoms. High androgen levels and insulin resistance are common in women with PCOS. Genetic factors play a role, although there is no specific “PCOS gene.” Studies suggest that hormone and insulin resistance genes can be inherited. PCOS can go unnoticed without symptoms until fertility issues or unexplained weight gain arise. Some individuals may have mild PCOS with subtle symptoms.
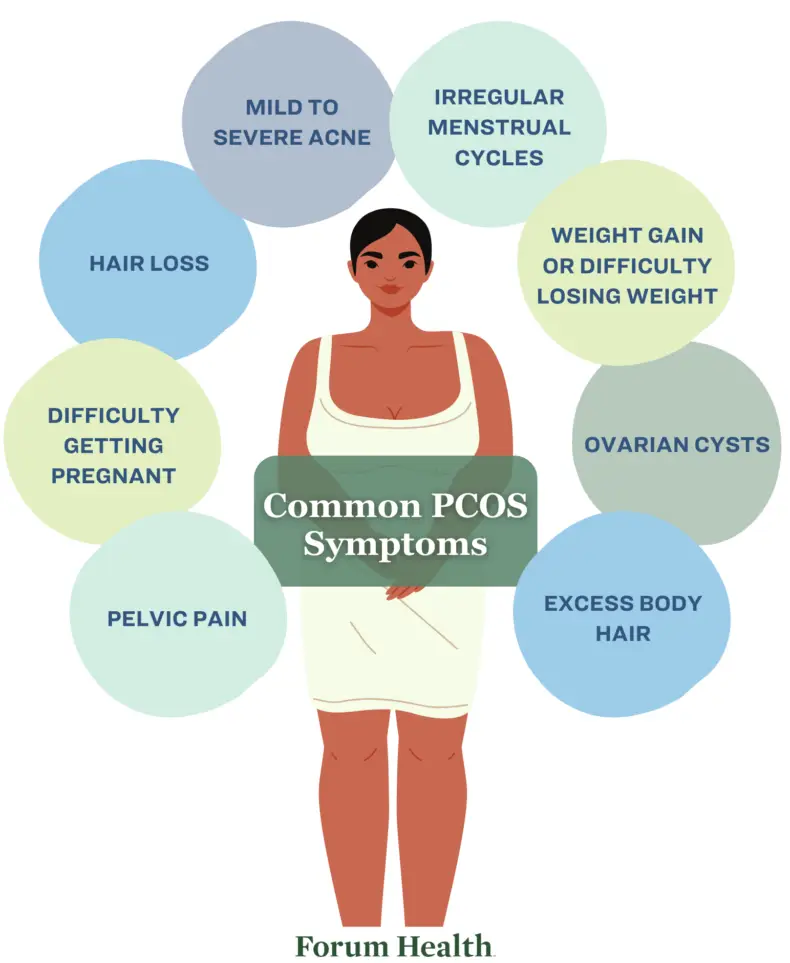
Symptoms of PCOS
- Irregular periods
- Absent periods
- Infertility
- Acne, excess body hair, and loss of hair on the scalp
- Insulin resistance
- Obesity
- Low progesterone levels
- Estrogen dominance
- Hypothyroidism
- Abnormal cholesterol, including high triglycerides
- Prediabetic A1C ranges
- Ovarian cysts
- Sleep apnea
- Skin tags on the armpits and neck area
- Dark patches of thickened skin, particularly on the neck, armpits, groin, and under the breasts
- Fatigue
- Thinning hair
- Mood changes
- Pelvic pain
- Depression
Do I have PCOS?
Take this free symptoms quiz to determine whether you could have PCOS.
Insulin Resistance
Up to 70% of women with PCOS have insulin resistance, a condition where your body doesn’t respond as it should to the hormone insulin.
When blood sugar levels rise after you eat, your pancreas releases insulin. This helps the glucose in your blood move into the cells in your muscle, fat, and liver, so they can use it for energy. But when you develop insulin resistance, the glucose stays in your blood instead of moving into the cells. To compensate, your pancreas secretes more insulin, and over time, your blood sugar levels go up.
Insulin resistance can cause weight gain, particularly around the abdomen. It can also lead to a wide range of problems, including metabolic syndrome and Type 2 Diabetes.
Estrogen Dominance
Another condition associated with PCOS is estrogen dominance, where the ratio between estrogen and progesterone is out of balance.
The lack of ovulation with PCOS produces continual levels of estrogen as eggs are released into the follicles. But because the eggs don’t mature, the body doesn’t produce adequate levels of progesterone. This throws off the ratio between estrogen and progesterone, which can contribute to PCOS and also cause abdominal weight gain, infertility, autoimmune disorders, and thyroid dysfunction. Estrogen dominance also increases the risk of endometriosis, breast cancer, diabetes, cardiovascular disease, and endometrial cancer.
How can we help?
Conventional treatment addresses the symptoms only with birth control and progestin pills, as well as pills to help with ovulation. As integrative medicine practitioners, we run a series of advanced tests, assess all the contributing factors, and work to create a plan that balances your hormones and puts you back in control.


